Comorbidities: Co-Occurring Mental and Alcohol Use Disorders
Comorbid mental disorders are common among people with alcohol problems. In Australia, of the 8841 people surveyed in 2007 for the National Survey of Mental Health and Wellbeing, 2.9 per cent met the criteria for harmful alcohol use, and 1.4 per cent met the criteria for alcohol use disorder (AUD). Of this latter group half (53.6%) met the criteria for an anxiety disorder and one-third (34.0%) met the criteria for an affective or mood disorder (ABS 2008). Other disorders associated with alcohol use disorder include other substance use disorders. Conversely, among people with mental disorders, such as depression, 34% of men and 15% of women have concurrent alcohol use problems. Exposure to trauma (such as witnessing serious injury or death, being involved in a life-threatening incident, or being threatened with a weapon etc) is very common among people with an alcohol use disorder. While people with post traumatic stress disorder (PTSD) are more than five times more likely to have an alcohol use disorder than people without PTSD only 5% of people with an AUD meet criteria for PTSD. Approximately one in five people with schizophrenia will have an alcohol use disorder at some time in their life. Thus, comorbid mental disorders are sufficiently common for their presence to be expected and their treatment planned for.
The following section is to be read in the context of the Australian national Guidelines for the management of co-occurring alcohol and other drug and mental health conditions in alcohol and other drug treatment settings (Marel et al., 2016). These national guidelines provide more advice and resources than is contained here. Additional assistance can be obtained from guidelines for specific disorders found in Appendix 5. To these resources, the following section provides specific information and recommendations about alcohol use disorders and adds research published since 2015.
Figure 21.1 shows guiding principles for working with people with comorbid alcohol use and mental disorders adapted from Marel et al (2016, p15).
Figure 21.1 Guiding principles for working with people with comorbid alcohol use and mental disorders
|
When working with clients with comorbid mental health conditions, it is recommended that health services and health professionals take the following principles into consideration as described throughout these guidelines:
-
-
As an individual health professional, work within your capacity (your scope of practice, or the bounds of your clinical competence) be realistic about what you can achieve, use the expertise of others, and coordinate care.
-
Recognise that the management of comorbidity is part of the core business of health care.
-
Provide equal of access to care.
-
Adopt a ‘no wrong door’ policy. The onus isn’t on the consumer of health care to understand how health services are organised nor for the consumer to know the best place to seek help, rather it is the responsibility of health care professionals to coordinate care and assist the person to receive optimal care.
-
Recognise that comorbidity is common and that all clients should be routinely screened for comorbid conditions.
-
Conduct ongoing monitoring of symptoms and assessment of client outcomes.
-
Adopt a client-centred approach.
-
Emphasise the collaborative nature of treatment.
-
Have realistic expectations, a non-judgemental attitude, and a non-confrontational approach to treatment.
-
Express confidence in the effectiveness of the treatment program.
-
Involve families and carers in treatment.
-
Consult and collaborate with other health care providers; and
-
Ensure continuity of care.
|
In discussing comorbid mental disorders, this section uses the terminology of the fifth edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013) or the World Health Organisation’s International Classification of Diseases, 11th edition because they provide specific criteria that define each disorder. These classifications are useful because they the most common classifications used in the research literature. Alcohol use disorder and the majority of the mental disorders are syndromes defined by characteristic patterns of reported symptoms and observed signs. Reported symptoms and observed signs are real, while syndromes are names to describe patterns of signs and symptoms that occur together, that have a common clinical course and that have some clinical utility. While underlying mechanisms that explain these symptoms and signs may be revealed by future research, these disorders remain descriptive syndromes.
Comorbidity presents diagnostic and management dilemmas. When a person first seeks assistance for an alcohol use disorder, motivation and engagement are crucial, as is gathering information and developing a shared understanding of the issues faced. Symptoms and concerns expressed in those initial contacts may demand immediate attention. With time it may become apparent that some concerns are the direct effects of intoxication or withdrawal from alcohol, and remit with abstinence or significant reductions in drinking. In other cases, mental disorders develop in parallel with alcohol use disorders. Still further cases show signs of mental disorders and alcohol interacting to cause greater problem severity, greater functional impact and poorer response to treatment. In addition, mental disorders may emerge or worsen in early abstinence from alcohol and may have been “masked” by alcohol. Differential diagnosis may be more important for longer term interventions - irrespective of how comorbidity developed initial management and treatment is usually similar.
Because comorbidity often implies a person has two related disorders, it may be better to consider multimorbidity both as a term and as a reminder to consider a broad range of health and related problems.
People with comorbid alcohol use and mental disorders should be offered treatment for both disorders as part of routine care. Interventions for people with comorbidity should be more intensive, as this population tends to be more complex and carries a worse prognosis than those with single disorders. Care should be taken to co-ordinate interventions so that they are integrated and complement each other.
Integration and coordination of care for people with comorbid alcohol use and mental disorders should occur at service or team level as well as within the care provided to individuals. Specialist services for people with alcohol problems need expertise in the assessment and treatment of comorbid mental disorders. People referred from one service to another sometimes don’t take up the referral (for a wide variety of understandable and legitimate reasons), and different services sometimes have different criteria for eligibility. In a siloed healthcare system, it is easy for people with more complex problems to “fall between the cracks”. Thus, to ensure the continuity of care, it is desirable to bring mental health expertise into alcohol treatment services rather than expecting people with comorbid disorders to cope with geographic, administrative and clinical differences between services. Guidelines advocating for integrated care for people with chronic and complex health conditions should be applied. Integration of the content of treatment is discussed in following sections.
Figure 21.2 illustrates the levels of integration of specialist drug and alcohol and mental health services. Depending on the relative severity of the alcohol use disorder and mental disorder, care can be provided in an appropriate specialised setting or in a primary care setting. As an example, the Victorian Guidelines for Alcohol and Drug Programs list comorbid mental disorders as one of the criteria for admission to subacute beds for withdrawal (VicHealth, 2018).
FIGURE 21.2: Level of care for people with co-occurring alcohol use and mental disorders
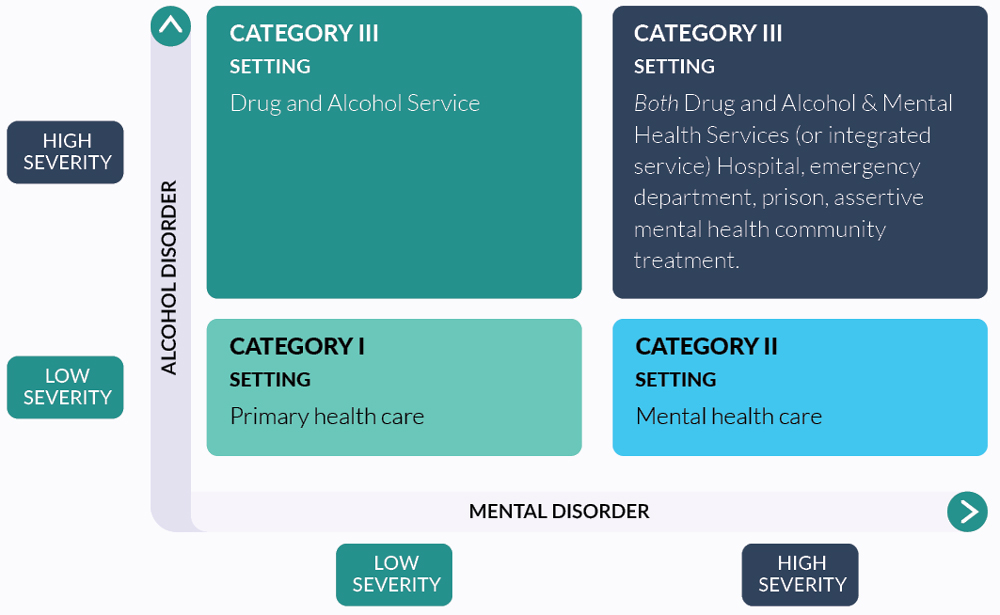
Note: Adapted from Center for Substance Abuse Treatment 2005. Substance abuse treatment for persons with co-occuring disorders. Treatment Improvement Protocol (TIP) Series 42, DHSS publication no. (SMA) 05-3922. Substance Abuse and Mental Health Services Administration, Rockville MD.
| Chapter |
Recommendation |
Grade of recommendation |
| 21.1 |
People with alcohol use disorder and comorbid mental disorders should be offered treatment for both disorders. Care should be taken to coordinate intervention. |
C |
| 21.2 |
More intensive interventions are needed for people with comorbid conditions as this population tends to be more disabled and carries a worse prognosis than those with single pathology. |
GPP |
| 21.3 |
At a minimum all Alcohol and other drugs (AOD) workers should be ‘comorbidity informed’, knowledgeable about the symptoms of the common mental disorders and how to manage these symptoms. |
GPP |